
On 8 January 2021 I began chemotherapy treatment at Brooks Army Medical Center in San Antonio, Texas.
The Treatment Begins
Before chemotherapy started I met with my oncologist nurse, Ms. Lisa to go over my therapy and have blood work done. This included genetic testing.
The results, my CA-125 tumor markers were sky high at 758. The goal is to get them <48. A CA-125 test measures the amount of the protein (cancer antigen 125) in your blood. This test is used to monitor certain cancers during and after treatment.
My results also revealed I was BRCA1 positive, which means I have the genetic mutation; I either got it from my mom or my dad. A positive test result means that I have a mutation in one of the breast cancer genes, there's BRCA1 and BRCA2, and therefore a much higher risk of developing breast cancer or ovarian cancer compared with someone who doesn't have the mutation.
So how do these 2 tests work together? I cannot stress how important genetic testing is. If you test positive for BRCA1 or BRCA2, a CA-125 test can be used to look for early signs of ovarian cancer in people with a very high risk of the disease. We should demand these tests to be started as early as age 25. Please, ask your doctor! You can also pay out of pocket for the genetic test. I think it's worth your life!
Treatment
Right now, my treatment plan is straight forward. I have 3 chemotherapy treatments, which consist of a 3 hour infusion of Paclitaxel (Taxol) followed by a 40 minute infusion of Carboplatin (Paraplatin). I go to treatment every 21 days.
Once I complete my first 3 treatments I will be evaluated and hopefully be ready for surgery. Surgery will consist of debulking and a full hysterectomy. It will also require a gastroenterologist surgeon to remove a section of my colon and put my colon back together. I'm hopeful I can wake up from surgery without any ostomy bags hooked to my abdomen. I am also hopeful that my oncologist will have a successful surgery.
What's next after surgery? As of right now, 3 more chemotherapy treatments. I fully understand that things may change. I also fully understand this will be a lifelong battle. My chances of reoccurrence is high due to my genetic mutation. I am also at risk of developing breast cancer. In this case, I am being proactive and meeting with surgeons to start planning a double mastectomy once I complete my OC treatments.
Chemo Treantments 1 & 2
So far chemotherapy has been working for me. My CA-125 levels went from the 700's to the 200's after my first treatment on 8 Jan. I'll get more bloodwork done on 22 Feb to see where they are now.
I've had bad reactions to Taxol both treatments but I'm willing to fight through it because I know my combination of infusions are working. My first reaction it felt like my face and neck were on fire 🔥 and I couldn't breathe. They stopped my infusion and started my at a slower drip rate. After that I was fine. My second treatment my reaction was a bit more intense. After 12 minutes of feeling fine after the infusion started all the sudden I felt burning and tightness in my chest, then it moved up to my neck. I don't know what a heart attack feels like, but I thought this was it. I was knowledgeable enough to know how to stop the infusion machine and just focus on my breathing. Last thing you want to do is panic. After 20 minutes they started the drip at a super slow rate. My oncologist sat with me to ensure I was okay for about 20 minutes. He did an awesome job distracting me. All was good!
3rd Chemo Treatment

Finally!!! This time around "ZERO" reaction to the Taxol. My nurse started the drip super slow this time. Started it at 50 ml/hr and worked our way up to 192. No issues at all!
I did bloodwork on Monday and the results are in. My tumor markers CA125 level dropped again. It went from 258 to 119. If you remember, I started at over 700 U/ml back in January. Normal levels are =/< 46 U/ml so I am getting there, today's chemo may just do that. Fingers crossed 🤞🏼
CT/PET Scan
Got my CT/PET scan today, 11 March in preparations for my surgery next week. The prep was pretty normal like any other scan, IV placed for the contrast. If you're good with CT scan, you'll be fine with a PET. It just takes a little longer to ensure the images are good. The reason for both CT and PET scan are the images are overlapped so the physician can see exactly what is going on and give them a better idea of their preparation and plan before surgery.
Results come Monday!

The silver ring is the CT scan portion. Then the back side is the PET scan portion
Surgery #2
Today is the day! 🍀💚🍀💚🍀

Surgery Day! Got on my green for luck. Happy St. Patrick's Day 🍀🍀🍀🍀
Day 1 After Surgery: In a butt load of pain. As to be expected. Full hysterectomy surgery went well and most if not all of the other malignant nodules were burned off. I haven't looked at the incision yet. It usually takes me until I get home to look at everything. While I'm here in the hospital I just let the nurses do what they need to do.
Woke up with one of my colostomy bags. The docs had to take out my dicending piece of colon and part of my rectum that had disease on it. Stoma Steve will be around a bit longer than expected. Wasn't too happy but I know they did what was best. After I recover from surgery and go through my chemo treatments we will re-attack. I'm left with 30% of my colon to work with.
Been pushing through the pain. Once I finally got ahead of it I changed into my own comfy clothes, brushed my teeth, washed my face, got out of that dreadful bed and took a walk around the floor. By dinner I was eating all my food.
GOAL: Get discharged Saturday!
Day 2 After Surgery: Woke up to nurses trying to drawl blood at 4am. After 4 pokes they finally were successful. My hands and arms are really bruised up. I've been pretty tired today. I ate a good breakfast; scrambled eggs, oatmeal and a banana 🍌. Colored a little in my Relaxation coloring book.
Next I need to get a blood transfusion because my hemoglobin level was low. One of the speed bumps holding me back from discharge. Plus when it's low I get really tired. Like I am now. It's hard just to type this right now.
Having a little pain today where my left side ostomy was closed. It currently looks ugly, but doctors assured me it will heal just fine.
Day 3 After Surgery: Woke up early again at 3:30am. This time my bladder woke me up and some mild pain. Knew I wanted to go home as soon as I got up. So today I got up the chair at 6am and walked the floor before lunch. I've been able to manage my pain from getting bad thank goodness.
My hemoglobin level went up to 7.1 after the morning blood work. After 2 liters of blood I swore my levels would go up higher. Dr. Phippen was surprised as well. They took another blood drawl at 1000 and that came up to 7.4. Since it was moving in the right direction I was able to go home.
Not much else happened today. I'm just super proud of myself for taking care of my body from last surgery so I could go home pretty quick this time. I was focused this time on what had to do to go home. In my comfy recliner now ready to fall asleep.
I was sent home with about 8 bottles of medicine and my injections and, of course, more colostomy bags. Now I just need to build myself up again for next surgery. 2 of 4 done!
Day 4 After Surgery: Not sure why this is happening but I'm in a lot of pain today. I've been taking the meds as prescribed, it just feels like nothing is working. I think I jumped the gun too quick leaving the hospital.
I woke up at 430am to come lay in my recliner. Feel asleep there until my alarm went off to take my first rounds of meds (Oxycodone, Tylenol, heart burn meds and thyroid med).
I was able to jump online with Survivors Teaching Students Zoom to introduce myself. Then my Home Nurse came by to get my services started back up. Now I'm back in my recliner about to fall asleep again.

First day in recovery. Was in a lot of pain. So glad I brought my own heating pad

Needed a blood transfusion due to low levels of hemoglobins. Thank you to all the blood donors out there!
Day 5 After Surgery: I felt much better today. Rested a lot. Finally removed bandages and took a really good shower. There was still some bleeding from the incision so I bandaged myself back up. Hopefully in a few days I can remove them permanently. I just have to be careful with my clothes rubbing the incision. There's no way to avoid it. This time it went down to my pubic hair. That's about 4 inches longer than last surgery. With this surgery rest is good. Over the next week I'm going to take it as easy as possible. Today I slept a lot but that's what I need to heal
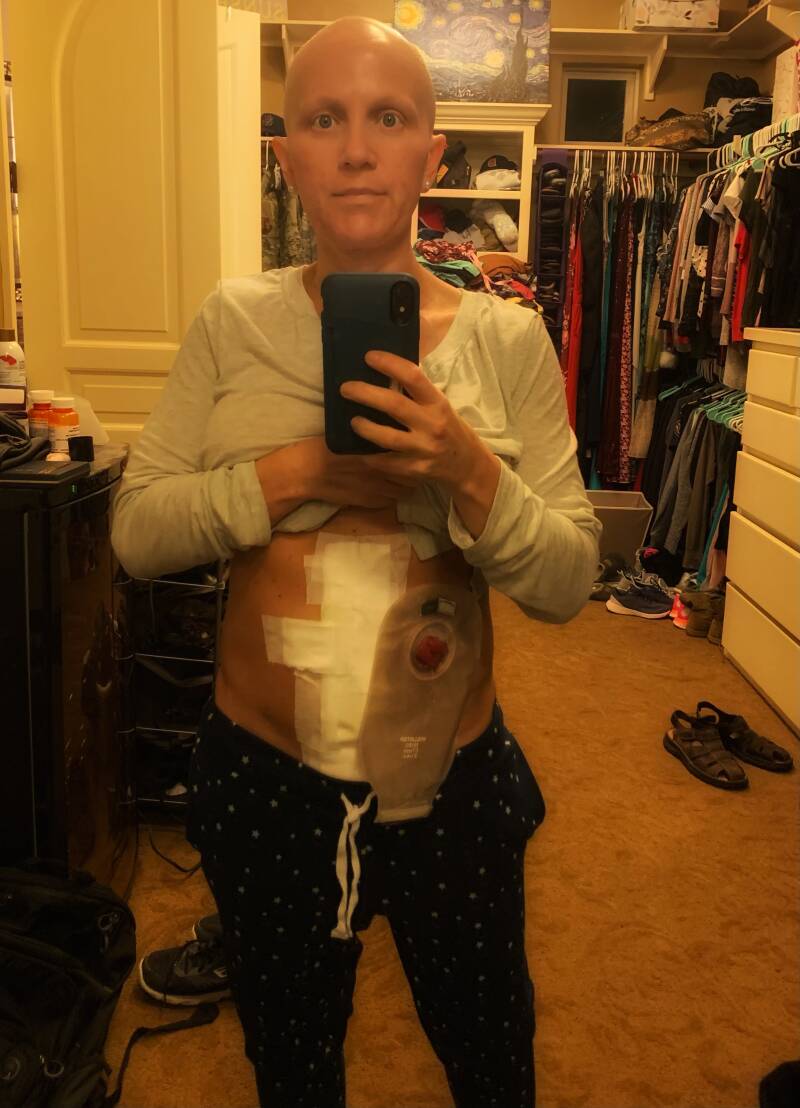
Day 10 After Surgery: I'm guessing you can see that the pain I was experiencing put me down for 5 days. It hasn't been a fun road at all. It's still there but it's getting manageable now. Only thing I'm concerned with is my stoma output. There's is no output but a bit of liquid. My last solid output was Friday, so I started drinking Miralax. Plus I'm eating more.
Yesterday Josh got me outside for a walk so hopefully I can do the same, if not more, today. Things are starting to look better. This recovery has been a beast.
Go to drop down under "Treatment Begins" for more pages about my unexpected surgery, final 3 chemo treatments & updates on my ostomy reversal